
COVID-19 can infiltrate insulin-producing cells within the pancreas, be taught about suggests
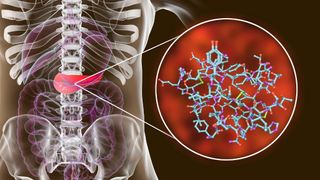
The coronavirus that causes COVID-19 can infect insulin-producing cells within the pancreas, lowering their capability to secrete insulin and barely causing cell demise, a brand contemporary be taught about suggests.
Hostile these insulin-producing cells, is named beta cells, can doubtlessly irritate indicators of diabetes, in particular form 1 diabetes, wherein the pancreas already makes shrimp to no insulin, essentially essentially based entirely on the be taught about authors. “Whenever you happen to imagine that there are some sufferers who have already got diabetes, if the virus is available in and nails the closing beta cells you’ve got, that is no longer merely,” stated co-senior creator Peter Jackson, a professor within the department of microbiology and immunology at Stanford University College of Remedy.
In addition to, some studies counsel that excessive COVID-19 could presumably well additionally trigger diabetes in of us and not utilizing a earlier historic past of the condition, as soon as more elevating the likelihood that the virus infects beta cells, Reside Science previously reported. This pattern remains to be being investigated, but given the contemporary knowledge, Jackson stated that he thinks the virus could presumably well additionally infrequently induce diabetes by injuring beta cells; this is in a position to be in all likelihood to happen when of us with prediabetes, or a range of effectively being stipulations that elevate the hassle of diabetes, make a excessive case of COVID-19.
Linked: 20 of the worst epidemics and pandemics in historic past
Of us with both form 1 or form 2 diabetes — where the physique makes some insulin however the tissue can’t shield it up attributable to insulin resistance — face a better effort of growing excessive COVID-19 indicators than the stylish population, essentially essentially based entirely on the Centers for Illness Defend watch over and Prevention (CDC). In stylish, of us with diabetes are more seemingly than those with out the disease to experience considerations when infected with any virus, since the condition can impair immune honest.
That stated, no one knew whether SARS-CoV-2, the virus that causes COVID-19, can straight assault the pancreas, Jackson stated.
To probe this demand, Jackson and his colleagues ran experiments on pancreatic tissue from organ donors, nine of whom had died from excessive COVID-19 infections and 18 who died of a range of causes and examined detrimental for the virus. Within the predominant community, they chanced on SARS-CoV-2 had straight infected the beta cells of some other folks, and in several lab dish experiments, they chanced on that the virus could presumably well additionally infect, anxiety and extinguish beta cells drawn from the a range of donors who died from non-COVID-19 causes, essentially essentially based entirely on a sage printed Would possibly perchance perchance also merely 18 within the journal Cell Metabolism.
Nonetheless, even with this contemporary evidence, the central demand of whether SARS-CoV-2 straight infects beta cells in vivo stays unsettled, stated Dr. Alvin Powers, director of the Vanderbilt Diabetes Middle in Nashville, who modified into as soon as no longer appealing with the be taught about. The contemporary be taught about presentations that pancreatic cells will be infected in a lab dish, however the same has no longer been definitively shown in other folks, he stated; to reach a solid conclusion, scientists will must envision many more pancreas samples from sufferers who died of COVID-19.
Virtually about the reports of COVID-19 triggering diabetes, “we know that those that have borderline diabetes, or prediabetes, as soon as they earn [critically] in melancholy health with something else, with pneumonia, with a heart assault, with a stroke … diabetes infrequently looks,” Powers knowledgeable Reside Science. So or no longer it is seemingly that there could presumably well additionally be uptick in diabetes conditions, “no longer thanks to snort toxicity from the SARS-CoV-2 virus,” but because significantly in melancholy health of us infrequently make diabetes. In stylish, reports of COVID-19-linked diabetes have been conflicting and mute warrant extra investigation, Powers wrote in a most contemporary commentary, printed April 7 in The Lancet.
How the virus could presumably ruin into beta cells
To search out out whether SARS-CoV-2 infects beta cells, the first step is to resolve out how the virus would infiltrate those cells within the predominant space.
The virus essentially uses a receptor protein known as ACE2 to sneak into cells, but several a range of proteins on the cell surface appear to attend high the virus to hobble into ACE2, Powers stated. For a most contemporary be taught about, printed Dec. 1, 2020, in Cell Metabolism, Powers and his colleagues went making an attempt for ACE2 and one of those proteins, known as transmembrane serine protease 2 (TMPRSS2), in beta cells, but chanced on shrimp of both. In one other independent be taught about, printed within the same journal, researchers reached the same conclusion, making it seem admire SARS-CoV-2 had few doorways into beta cells.
“The controversy comes from, ‘Hi there there is no longer so noteworthy receptor right here, so it must no longer be that the virus infects beta cells,'” stated co-senior creator Raul Andino, a professor within the department of microbiology and immunology at the University of California, San Francisco. Nonetheless, there is a requirement as to how noteworthy ACE2 the virus desires to ruin into cells, and mute a range of proteins could presumably well additionally attend enhance its capability to latch onto the ACE2 receptor, Andino stated.
As an illustration, receptor proteins known as neuropilin 1 (NRP1) and transferrin receptor (TFRC) have each and each been linked to SARS-CoV-2 infection; usually, the damaged-down binds to a range of thunder elements and the latter helps import iron into cells, but studies have chanced on that each and each receptors could presumably well additionally be exploited by the coronavirus. The crew seemed for these proteins, to boot to ACE2 and TMPRSS2, in beta cells from five COVID-detrimental organ donors.
“We isolate islets [groups of pancreatic cells] from human cadavers as they arrangement in,” Jackson stated, noting that the tissue ought to mute be silent and frequent immediate to be precious for experiments.
As in earlier studies, they chanced on low ranges of ACE2 and TMPRSS2 in beta cells from the donors, but apparently, they chanced on an abundance of NRP1 and TRFC. When put next with alpha cells, one other form of pancreatic cell, beta cells expressed noteworthy more NRP1 and TRFC, hinting that the virus could presumably portray a selectivity for the beta cell if it does infect the pancreas.
Linked: Why COVID-19 kills some of us and spares others. Here’s what scientists are discovering.
The crew then isolated more islets from COVID-detrimental donors and exposed the tissue to SARS-CoV-2 within the lab. After several days, they exposed the cells to antibodies that latch onto piece of the coronavirus, to envision which cells had been infected, and chanced on evidence of SARS-CoV-2 mostly in beta cells. They chanced on that they’re going to additionally considerably block this infection by blocking off the NRP1 receptor with a shrimp molecule known as EG00229. This reality hints that NRP1 could presumably well additionally be key to the coronavirus coming into beta cells, Jackson stated.
“Take into consideration you are making an attempt to shield a basketball: A one-handed shield is refined and … you flub the ball plenty of the time. A two-hand shield is a much more merely and environment pleasant event,” he stated. To contaminate cells, a building on the coronavirus known as the spike must hobble into ACE2; on this analogy, NRP1 could presumably well additionally be serving to to “shield” the coronavirus and insert the spike, despite there being relatively few of ACE2 receptors available, he explained. Some studies counsel that NRP1 grabs onto a particular fragment of the spike, and that blocking off this interplay considerably hobbles the virus’s capability to contaminate cells in tradition, essentially essentially based entirely on a November sage within the journal Science.
The crew also chanced on that infected beta cells produced vastly less insulin than uninfected cells when exposed to a meal’s price of glucose; and in infected cells, molecular indicators linked to cell demise started to spike. These outcomes could presumably well additionally as soon as more be blocked with EG00229, underscoring the doable significance of NRP1 to infection.
After seeing that the virus could presumably well additionally infect beta cells from COVID-detrimental donors, the crew critical to envision if the virus cropped up in those that had died of COVID-19. They chanced on coronavirus genetic area subject in seven out of the nine donors’ pancreases. The utilization of antibodies, as within the earlier experiments, the crew confirmed that SARS-CoV-2 seemed in four out of the seven donors’ beta cells; interior those beta cells, to boot they chanced on genetic instructions coding for the spike protein.
The a range of three donors’ pancreases showed in depth anxiety, resulting from digestive enzymes that immediate employ away at the organ after demise, the authors notorious of their sage. So it will additionally be that the antibody take a look at came aid detrimental for 3 donors attributable to the severity of that anxiety, Jackson urged. On the a range of hand, the detrimental tests could presumably well additionally be merely, as no longer all sufferers with excessive COVID-19 necessarily have infected beta cells.
“We would in level of reality must vitality a noteworthy better be taught about to earn a proper number as to the infection rate in pancreatic beta cells for sufferers with excessive COVID,” Jackson stated.
The be taught about raises a range of questions. Assuming the virus attacks beta cells in living of us as it does in lab dishes, how does the virus first reach the pancreas? The onset of pneumonia could presumably well additionally attend the virus ruin out the airways and trigger secondary infection some other put, equivalent to within the pancreas, but for now that is unclear, Jackson stated. The be taught about also handiest incorporated of us with excessive disease, so or no longer it is unclear whether pancreatic infection ever takes space in gentle COVID-19 infections.
And if and when the virus pervades the pancreas, “how does infection of the pancreas correlate with … decreases in insulin?” Andino stated. The crew observed that within the lab dish, beta cells produced less insulin after infection, however the extent of that lower could presumably well additionally be a range of in a living particular person. “I mediate that is a serious demand, obviously … and that’s the explanation something to me that the paper does no longer deal with.”
In addition to, more study will be critical to be conscious the honest of the immune machine in pancreatic infection, he notorious. In theory, snort infection could presumably well additionally trigger in depth irritation within the pancreas, causing extra anxiety, and in of us inclined to form 1 diabetes, this is in a position to presumably well additionally trigger or irritate the autoimmune assault on the the organ. But for now, that is all speculation, Andino stated.
Given the boundaries of the lab dish be taught about, researchers need gigantic studies of effectively-preserved pancreases from those that died COVID-19 to substantiate the organ is straight infected, Powers stated. “Whether or no longer their methodology to infecting cells mimics what happens when an particular person has SARS-CoV-2 infection is no longer obvious.”
Initially printed on Reside Science.