
In some unspecified time in the future of the Slump to Hold a Larger $500 Emergency Ventilator
Because the coronavirus crisis lit up this spring, headlines about how the U.S. might per chance well moreover innovate its intention out of a pending ventilator shortage landed nearly as arduous and immediate because the pandemic itself.
The Fresh Yorker featured “The MacGyvers Taking on the Ventilator Shortage,” an effort initiated now no longer by a doctor or engineer but a blockchain activist. The College of Minnesota created an economical ventilator called the Coventor; MIT had the MIT Emergency Ventilator; Rice College, the ApolloBVM. NASA created the VITAL, and a effectively being visual show unit firm got in the game with Fitbit Float. The mark tags varied from $150 for the Coventor to $10,000 for the Fitbit Float — all vastly lower than top class commercially on hand health facility ventilators, that will bustle $50,000 apiece.
Around the identical time, C. Nataraj, a Villanova College of Engineering professor, changed into hearing from entrance-line clinical doctors at Philadelphia hospitals petrified of working out of ventilators for COVID-19 patients. Compelled to support, Nataraj attach together a volunteer SWAT team of engineering and clinical expertise to scheme the supreme emergency ventilator. The aim: fabricate one thing that might per chance well moreover operate with as a minimum 80% of the characteristic of a conventional health facility ventilator, but at 20% or much less of the price.
For a long time, Nataraj has worked on clinical projects — treasure finding a greater strategy to diagnose a doubtlessly deadly brain break in premature infants — essentially with clinical doctors at Young of us’s Sanatorium of Philadelphia and the Geisinger Health system in rural Pennsylvania, so key clinical avid gamers came together . By March 23, he had approached engineering college about participating on a monthslong effort to manufacture the NovaVent, a overall, low-mark ventilator with parts that mark about $500. The schematics would be birth-sourced, so others might per chance well moreover use them free of mark to mass-accomplish the instrument.
The Fresh Yorker wasn’t by myself in referencing the ’80s TV series “MacGyver,” whose protagonist changed into a Swiss Navy knife-carrying undercover agent who got the job completed with wits and no topic changed into at hand. The recommendation changed into that these ventilators had been straightforward ample to throw along with parts from a clinical present closet or your neighborhood hardware retailer. “Each person can accomplish it,” one headline be taught, enticingly. These miracle machines, the thinking went, will be advisable in U.S. hospitals dealing with extreme shortages, per chance in cities surging with sick patients.
To treasure the aptitude utility and appropriate charges of these emergency ventilators, KHN adopted Villanova’s team for three months as it developed, tested and ready to submit the NovaVent for Food and Drug Administration approval.
The team tapped a maker of car parts, along with roboticists. It gathered enter from anesthesiologists as effectively as electrical, mechanical, fluid systems and laptop engineers. It tapped nurses to support be sure users would at once know how chances are high you’ll well per chance operate the ventilator. Local manufacturers 3D-printed items of the machine.
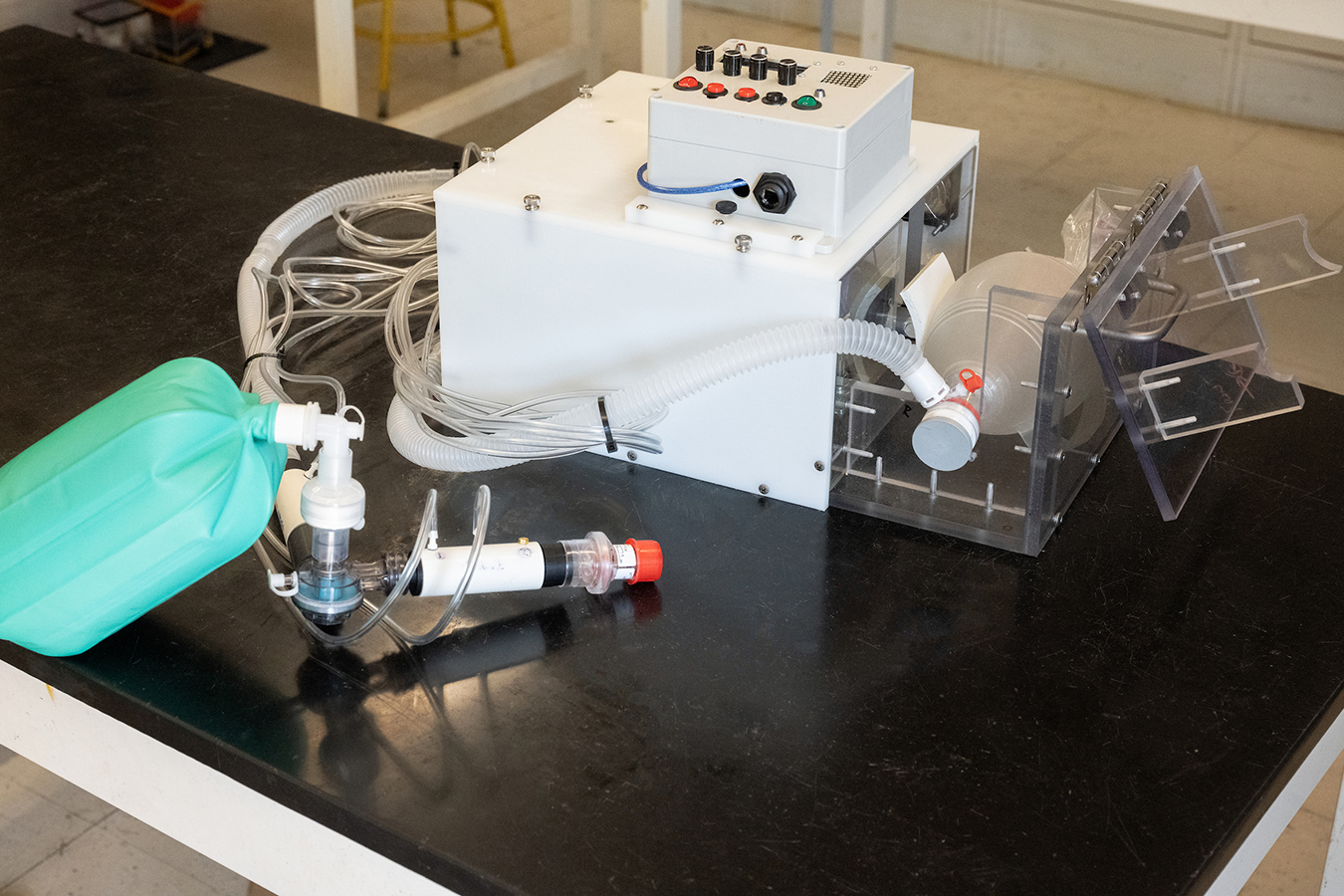
When the pandemic emerged, a Villanova engineering professor gathered a volunteer SWAT team of engineering and clinical expertise to scheme an emergency ventilator that supplies as a minimum 80% of the characteristic of a conventional health facility ventilator, but at 20% or much less of the price. The completed NovaVent prototype is displayed at the Villanova College of Engineering on June 3.(Villanova College/Paul Crane)
Nataraj and his team realized that a pair of of the assorted ultra-bare-bones machines wouldn’t meet the criteria of the recent U.S. effectively being care system. Nonetheless they moreover believed there changed into heaps of room for Villanova’s team to innovate between these and the high-cease, costly gadgets from companies treasure Philips or Medtronic.
One direct is apparent: The $500 ventilator is one thing of a unicorn.
While the parts for the NovaVent mark about that great, the brainpower and of us hours added uncounted price. Within the early phases, the core community — all volunteers — worked 20 to 25 hours every week, Nataraj mentioned, mainly by strategy of Zoom calls from home on high of their day jobs.
Groups of two or three had been allowed into the lab to work — almost about essentially the easiest of us on campus. The direct, in spite of the complete lot, changed into in step with the college’s Augustinian mission, which values the pursuit of files, stewardship and neighborhood over the person.
By the time they realized what they might per chance moreover fabricate with the $500 model, the predominant wave of crisis had handed. But in these weeks, an alarm resounded finally of the land about the unpleasant tell of America’s public effectively being system.
So the NovaVent mission pivoted: fabricate greater low-mark vents for hospitals in depressed and rural U.S. communities that contain few, if any, ventilators.
One immediate legacy of the innovation occurring at Villanova and elsewhere is the final public-spicy nature of the danger, mentioned Dr. Julian Goldman, an anesthesiologist at Massachusetts General Sanatorium who helps location requirements for clinical gadgets: “Of us from varied walks of life in the case of their expertise — engineers, clinicians, pure scientists — all thinking and dealing to utilize a glimpse at to pick out how chances are high you’ll well per chance pass in a short time to resolve a national emergency with many dimensions: How will we accomplish the affected person safer? How will we accomplish the caregiver safer? How will we take care of present chain boundaries?”
From varied ventures, recent designs contain already been ragged as a leaping-off show conceal fabricate emergency ventilators in a foreign country. They’ve moreover bolstered Fresh York City’s stockpile and might per chance well moreover add to tell and national reserves as effectively.
The early, pressing considerations a pair of looming ventilator shortage had been effectively based: On March 13, the U.S. had about 200,000 ventilators, based utterly on the Society of Important Care Drugs. Nonetheless thanks to the surge of COVID patients, it changed into predicted the country might per chance well moreover soon want as many as 960,000.
We mentioned, ‘Smartly, GM is making it. Why are we making it?’ Nonetheless there changed into heaps of uncertainty with the epidemiological units. We didn’t know how adversarial it changed into going to score. Or [the curve] might per chance well moreover entirely fall down and there’d be no want the least bit.
In early April, Fresh York Gov. Andrew Cuomo mentioned the tell would bustle out of ventilators in six days, leaving clinical doctors with the originate of grim calculation they’d heard about from arduous-hit northern Italy: “If a particular person comes in and desires a ventilator and besides you don’t contain a ventilator, the actual person dies.”
In Philadelphia, 12 miles east of Villanova, health facility directors braced for shortages and reported short supplies of the medication required to sedate patients on ventilators.
President Donald Trump invoked the Defense Manufacturing Act to score predominant manufacturers to accomplish ventilators, even supposing GM changed into already engaged on it. When GM signed a $500 million contract to bring 30,000 ventilators to the U.S. government by August, the NovaVent team wondered whether or now no longer its contain efforts would be futile.
“We mentioned, ‘Smartly, GM is making it. Why are we making it?’” Nataraj mentioned. “Nonetheless there changed into heaps of uncertainty with the epidemiological units. We didn’t know how adversarial it changed into going to score. Or [the curve] might per chance well moreover entirely fall down and there’d be no want the least bit.”
And for a pair of weeks, it did seem the worst changed into over. The price of newest circumstances began to tiring in the nation’s early epicenters. Hot spots flared in nearly every pocket of the country, but these too had been mostly contained.
Of us spilled lend a hand into long-established life, gathering in backyards, seashores and bars. In June, records coverage moved on to the calls for racial justice and mass protests after the videotaped killing of George Floyd in the custody of Minneapolis police.
Within the background, the highly contagious coronavirus tore finally of the South, thru Florida, Georgia, Texas and Arizona, and surged in California. Some states reported ICU beds had been rapid at or above ability. This rapidly virus had proved uncontrollable, and the prospect of ventilator shortages had bubbled up once extra.
Past pandemics were mothers of innovation. Development in mechanical ventilation started in earnest after a 1952 polio outbreak in Copenhagen, Denmark. Basically based on the American Journal of Respiratory and Important Care Drugs, 50 patients a day arrived at the Blegdams Infectious Illness Sanatorium. Many had stupefied respiratory muscle tissue; nearly 90% died.

Villanova engineering professor C. Nataraj stands with the completed prototype of the NovaVent ventilator at the Villanova College of Engineering on June 3. It changed into efficiently tested on an artificial lung at Young of us’s Sanatorium of Philadelphia on June 12.(Villanova College/Paul Crane)
An anesthesiologist at the health facility realized patients had been death from respiratory failure in preference to renal failure, as changed into beforehand believed, and advised forcing oxygen into the lungs of patients. This worked — mortality dropped to 40%. Nonetheless one wide direct remained: Sufferers had to be “hand-bagged,” with extra than 1,500 clinical students squeezing resuscitator baggage for 165,000 total hours.
“They’d recruit nurses and clinical students to face there and squeeze a rep,” says Dr. S. Put Poler, a Geisinger Health system anesthesiologist on the NovaVent team. “As soon as in a while they had been good so exhausted that they would tumble asleep and cease ventilating. It changed into obviously a catastrophe, so that changed into the inducement for growing mechanical ventilators.”
The first ones had been straightforward machines, great treasure the well-known emergency-use ventilators created all the intention thru the COVID crisis. Nonetheless these came with hazards akin to detrimental the lungs by forcing in too great air. More sophisticated machines would bring greater control. These engineering marvels — the screens, the assorted modes of ventilation, the slick touch-show conceal conceal controls designed to minimize the threat of break or error — improved affected person remedy but moreover drove charges sky-high.
The emergency ventilators of 2020 centered on units that, in most cases, ragged an Ambu rep and a few originate of mechanical “arm” to squeeze it. Most of us are mindful of Ambu baggage from scenes in TV programs treasure “ER” the place paramedics compress the manual resuscitator baggage to support patients breathe as they’re rushed interior from an ambulance. The baggage are already widely on hand in hospitals, mark $30 to $40 and are FDA-authorised.
Nonetheless making machines that are that uncomplicated might per chance well moreover render them effectively unnecessary (or, worse, unpleasant). Health workers watching college and health facility groups coalesce finally of the country this spring to originate low-mark emergency ventilators took seek — and afflicted.
They glimpse at one thing and issue, effectively, this might per chance’t be that tricky to manufacture. It good blows air. ‘I’ll utilize a vacuum cleaner and switch it on reverse. … It’s a ventilator!’
Goldman, the Massachusetts General anesthesiologist, changed into amongst the clinical examiners anxious about the complete slapped-together ventilators.
“We had the maker neighborhood being stood up in a short time, but they don’t know what they don’t know,” mentioned Goldman, chair of the COVID-19 working community for the Affiliation for the Advancement of Medical Instrumentation, the predominant source of requirements for the clinical instrument trade. “There had been movies of harebrained tips for constructing ventilators online by of us that don’t know any greater, and we had been very concerned about that.”
The general public doesn’t in spite of the complete lot perceive the nuances required to manufacture a score clinical instrument, Goldman mentioned.
“They glimpse at one thing and issue, effectively, this might per chance’t be that tricky to manufacture. It good blows air,” he mentioned. “‘I’ll utilize a vacuum cleaner and switch it on reverse. … It’s a ventilator!’”
AAMI wished to lend a hand innovation, but moreover security. So Goldman assembled a meeting of 38 engineers, regulators and clinicians to rapid write boiled-down guidelines for emergency-use ventilators.
The biggest ventilators had been based utterly on the root of a piston in a car engine, Poler mentioned: Build a piston on a crankshaft, hook it up to a motor and use a prance or “arm” to compress the Ambu rep.
“It’s greater than no ventilator the least bit, but it goes at one tempo. It doesn’t in spite of the complete lot contain any controls,” Poler mentioned — now no longer supreme when patients might per chance well moreover mute be monitored for adjustments in how their lungs are responding, or now no longer, to remedy.
Villanova’s team of engineers, clinical doctors and nurses realized that essentially the easiest ventilators, the ones that AAMI changed into concerned about, seemed as if it would ignore some overall, sensible considerations: What originate of hospitals would these be ragged in, and beneath what stipulations? What kinds of patients would be attach on these ventilators? For how prolonged? Would they be ragged as backups for elevated-cease ventilators? What about error alarms?
All lawful questions, Poler mentioned, but the respond to all of them in actuality is “we hope to never use these.”
Their most efficient use? “A surge direct the place you merely don’t contain ample of the mild ventilators.”
In space of disappear utterly bare-bones, the Villanova team designed the gadgets as even supposing they would one day be deployed in recent effectively being care.
Float sensors, which visual show unit affected person ventilation, mark quite rather a lot of hundred dollars, so the team designed its contain in the lab and 3D-printed it at a mark of 50 cents, Nataraj mentioned, enabled by strides in 3D-printing expertise that contain vastly sever the price of so many gadgets. Southco, a Pennsylvania-based utterly world manufacturer that makes parts treasure the latch for your car’s glove box, changed into tapped to use its 3D printers to accomplish airflow tubes and couplings for the ventilator.
Garrett Clayton, director of Villanova’s Center for Nonlinear Dynamics and Lend a hand watch over, changed into the day-to-day keeper of the prototype. He changed into in particular concerned about the addition of a take care of, which made it easier for him, and in a roundabout intention others, to lug the 20-pound instrument from the lab to home and lend a hand.
Clayton’s computerized control system measures the waft price of air going into the affected person and converts it into volume, great as commercial ventilators fabricate. That controls how arduous and immediate the Ambu rep is squeezed; it’s made from a curiosity-grade Arduino microcontroller board. A voice-newest motor linked to a linear actuator with a fist-formed share of PVC on the tip pushes the rep in and out. The operator of the ventilator can control the respiratory price (the option of breaths per minute), as effectively because the ratio between inspiration and expiration and the volume of air going in.
While broken-down ventilators contain many control solutions, Clayton’s team centered on good one: how great volume is compelled into the airway. “Now we contain a location point so we don’t break the lung,” he mentioned.
Polly Tremoulet, a analysis psychologist and human factors consultant for ECRI and Young of us’s Sanatorium of Philadelphia, changed into pulled in to focal point on error messages and be sure that the ventilators’ buttons and shows “spoke the shopper’s language,” whether or now no longer that consumer changed into an anesthesiologist in Fresh Jersey or a nurse in India pulled into an ICU COVID ward.
Graduate pupil Emily Hylton and varied nursing students had been introduced in to originate feedback about the use of the NovaVent and ask questions akin to: Would the complete controls and screens glimpse familiar to nurses at the bedside?
The very prospect of these low-mark gadgets is slightly recent, Nataraj mentioned, thanks to the price of microcontrollers with any right ability: “Twenty years ago, they mark, oh gosh, $20,000 — and now they’re $20.”
By Would possibly per chance per chance per chance moreover 30, the predominant NovaVent prototype changed into total. It changed into efficiently tested on an artificial lung at Young of us’s Sanatorium of Philadelphia on June 12. Villanova has applied for a patent for the NovaVent, to support accomplish certain it won’t be commercialized by others.
“Whenever you occur to accomplish it free without having a patent, varied of us can put it to use and price for it,” Clayton mentioned. “A patent protects the beginning-source nature of it.”
As soon as a provisional patent is got, the team will submit the ventilator for Emergency Use Authorization from the FDA — hewing to the rules location up by AAMI.
Within weeks of kicking off the NovaVent mission, the curve in the East Waft had indeed flattened, and states had ample no longer recent ventilators to treat every affected person. The life-threatening ventilator shortage had now no longer materialized. One of the vital crucial emergency-use ventilators based utterly on designs by varied groups, treasure the one at MIT, did disappear into manufacturing — but even these didn’t cease up in hospitals, and as a change went into city stockpiles supposed to minimize seemingly future reliance on the federal government. So the Villanova team seized on a recent, world mission.
“We thought if it wasn’t critical in the U.S. market,” Nataraj mentioned, “everyone is aware of the setting up world, in particular sub-Saharan Africa, Latin America and Central America, they don’t contain the identical roughly products and services that we fabricate here.”
Exact now, in Pakistan or in any low-resource country, a family member is hand-ventilating a child. Forward of COVID and after COVID, here’s an argument.
The place the ventilators might per chance well moreover cease up remains to be considered. Early on, Pennsylvania showed curiosity in serving to Villanova get manufacturing companions. The team has spoken with engineers in India, Cambodia and Sudan (which reportedly has easiest 80 ventilators in the complete country) who’re drawn to per chance finding a model to accomplish the NovaVent.
Six thousand emergency ventilators based utterly on the invent by the College of Minnesota were manufactured in the U.S., based utterly on Dr. Stephen Richardson, a cardiac anesthesiologist who worked on that mission. Three thousand had been made by North Dakota aviation and agricultural manufacturer Appareo for tell emergency stockpiles in North Dakota and South Dakota. UnitedHealth Neighborhood equipped $3 million in funding to accomplish one other 3,000 units made by Boston Scientific, which were donated to worldwide locations treasure Peru and Honduras thru U.S. organizations; others had been sent to the U.S. government.
Enjoy the Villanova team, Richardson mentioned he thinks essentially the most promising seemingly for these ventilators is in setting up worldwide locations.
“As soon as we had been arranging to score these donated to Honduras, we had been speaking with a doctor who changed into telling me that [at] his health facility appropriate now, the med students are good hand-ventilating patients. For the complete lot, and for COVID namely,” Richardson mentioned. “Exact now, in Pakistan or in any low-resource country, a family member is hand-ventilating a child. Forward of COVID and after COVID, here’s an argument.”
For Poler, the mission changed into a reminder that the country needs to are inclined to its stockpiles. “Of us had been concerned about [ventilator reserves] in the ’90s, and then they on the complete quit concerned about it,” he mentioned. “COVID is a beautiful reminder that we shouldn’t contain stopped concerned about it.”
Goldman mentioned the national efforts might per chance well moreover now no longer result in a flood of cheap ventilators in U.S. hospitals. World use might per chance well moreover moreover be tricky. In worldwide locations with few resources, even very low-mark ventilators might per chance well moreover now no longer be seemingly thanks to lack of electricity or compressed oxygen, even supposing there is “doubtlessly a candy space of want and functionality the place these items will be deployed.”
On the upside, he mentioned, the pandemic kicked off a nearly phenomenal world engineering effort to allotment records and resolve the difficulty.
“If there’s going to be a magic bullet to arrive lend a hand out of this, it’s going to be the aptitude of our communities and our infrastructure,” he mentioned. “Of us stood up, attach in the valid processes and spirit, worked arduous, made it occur. We’ve added resilience to the effectively being care sector. That’s the final result here.”
As for the NovaVent, team individuals had been relieved they didn’t want to speed it into manufacturing as COVID-19 changed into ripping thru the Northeast this spring, thanks to aggressive efforts to flatten the curve. “We ended up without a ventilator shortage, which can be very good,” Clayton mentioned. “Nonetheless with the magnify in circumstances now, it’s very that chances are high you’ll well per chance issue of a pair of of them might per chance well moreover score ragged.”
To manufacture on the mission, Villanova is elevating money for a laboratory for cheap clinical technologies called NovaMed. The lab formalizes the formula of making cheap clinical instruments that follows the 80-20 characteristic-to-mark rule. The college says the lab is “motivated by the thought that earnings might per chance well moreover mute now no longer pick who has score entry to to lifesaving care.”
The direct to stop a ventilator shortage, Nataraj mentioned, made him issue extra critically about the American effectively being care system total.
“How arrive we haven’t built the expertise, the industrial and social systems that are in a space to home a direct treasure this — in particular when one thing treasure this changed into predicted?” he mentioned. “It’s absolute nonsense. Why might per chance well moreover mute a single particular person die in consequence of we weren’t willing?”
Related Issues
Cost and Quality Health Care Costs Health Exchange Public Health
COVID-19 Disparities