Op-Ed: RAS Imbalance Is COVID’s Razor
Occam’s Razor posits that “the finest clarification is in general elegant.” With COVID-19 the finest clarification is that the coronavirus strikes one cell purpose nonetheless does so in in point of fact every organ and tissue within the human body, such that a single mechanism underpins all coronavirus outcomes. To manufacture this, the aim must restful be a cell pathway that impacts nearly every bodily procedure.
COVID-19 defied public expectations of a flu-esteem respiratory illness, and as a change equipped something unpredictably menacing. A maelstrom of unexpected coronavirus concerns at a loss for phrases the clinical neighborhood, from renal failure to still hypoxia, from hyperglycemia to lack of olfactory sensation, from a Kawasaki-esteem myocarditis syndrome in young folk to blood clots and strokes in young adults.
Simultaneously dysregulating blood clotting and gastrointestinal feature, unfavorable kidneys and lungs, perturbing neuronal processes and immunological feature, the coronavirus regarded to be disrupting myriad cell pathways concurrently. Nevertheless that would indicate that a little RNA virus, incapable of even replicating itself independently, can salvage a staggering array of disruptive cell actions.
RAS, the renin-angiotensin procedure, is neatly identified as a circulating corrective mechanism, restoring blood stress and blood volume in the match of hemorrhage or dehydration. Nevertheless RAS is additionally a pervasive regulator of myriad tissue-stage functions, ranging across the spectrum of bodily programs: glucose metabolism, cardiovascular functions, hypoxia sensing, neural crosstalk, inflammatory response, coagulation, and more.
All over stress response to severe injury, the precedence is re-organising physiologic homeostasis neatly suited with survival and that requires integrated responses by nearly all organ programs. Evolution made RAS the master regulator coordinating these processes.
The classical depiction of RAS is a linear cascade of enzymatic activations, initiating with angiotensinogen conversion to angiotensin I (AI) by renin, adopted by AI conversion to angiotensin II (AII) by ACE. This sequential pathway is is known as “the ACE axis.” AII binds the AT1 receptor, initiating its multiple outcomes, including renal sodium conservation, coagulation, inflammation, fibrotic repair, and cell loss of life.
RAS comprises additional ingredients that counterbalance the ACE axis. The AT2 receptor provides an alternative for AII binding, yielding anti-coagulation, anti-inflammation, and anti-fibrosis outcomes. And ACE2, a “younger brother enzyme” to ACE, metabolizes AII, so that it’s unavailable to bind AT1.
ACE2 converts AII into an anti-inflammatory counterpart called A1-7. ACE2 additionally diverts AI out of the ACE axis, converting AI to an anti-inflammatory precursor, A1-9, thereby stopping introduction of AII. Thus, “the ACE2 axis” decreases activation of AT1 by AII, and acts as a counterweight to the ACE axis. RAS is now no longer linear as a minimum, nonetheless reasonably a web-based of interlinked enzymatic processes.
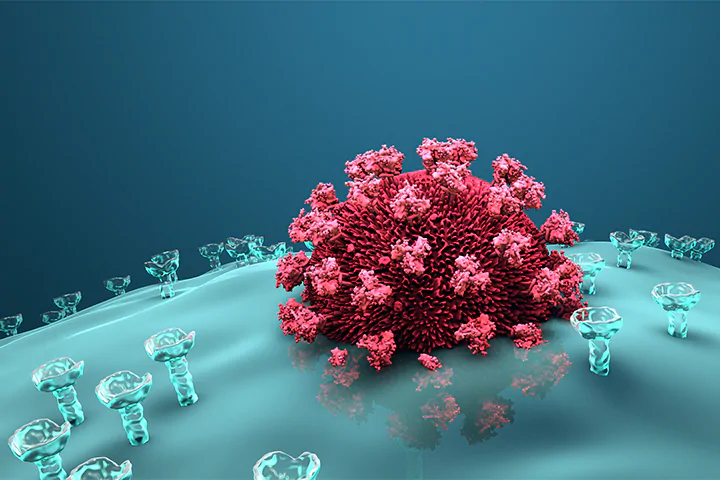
SARS-CoV-2 enters cells by binding cell-floor ACE2, touring as an uninvited visitor when a cell remembers ACE2 to its internal. As soon as internal, coronavirus shuts down cell production of ACE2, leaving the ACE axis working amok.
AII overproduction by unbalanced ACE triggers unnecessary coagulation resulting in blood clots and strokes; it provokes inflammation and fibrosis that nervousness renal tissue and promote arrhythmias. And it disables glucose-regulating functions of the insulin receptor, resulting in hyperglycemia and diabetes.
AII additionally disrupts cell volume regulation and triggers tainted cell loss of life, each of that can also indicate carotid body failure to register hypoxemia, resulting in still hypoxia, as neatly as lack of olfactory neurons, which disables sense of scent.
COVID-19 is deadly due to it targets the RAS master-regulator, and there shouldn’t be a backup quarterback. Multiple organ functions spiral into disarray, as SARS-CoV-2 turns the guardian of our evolutionary survival against us.
Importantly, many population subsets demonstrating worse COVID-19 outcomes voice a pre-gift RAS imbalance, with elevated ACE activity and diminished ACE2 counterweight, before ever encountering SARS-CoV-2. These encompass folk with diabetes, folk with hypertension, folk who smoke nicotine products, folk with weight problems, obvious cancer sufferers, males, and older adults.
As well, there is evidence that some African People and Hispanics can also carry genetic predisposition to RAS imbalance, attributable to former evolutionary pressures from water and sodium scarcity in tropical climates.
In essence, coronavirus pushes organ feature in the direction of a cliff by downregulating ACE2; nonetheless high-likelihood folk who regain baseline ACE overactivity and low ACE2, initiate up closer to that cliff, and thus usually are usually pushed over it by the virus.
This doesn’t indicate that RAS imbalance is the finest ingredient accountable for COVID-19 severity. Other folks with diabetes, cancer sufferers, older adults, and folk with weight problems regain demonstrable dietary deficiencies and immune impairment. Males regain acknowledged variations in immune feature compared to females, and males on the whole regain elevated charges of smoking.
Socioeconomic disadvantages had been rightly emphasised when assessing mortality disparities breaking alongside ethnic lines.
Yet the fingerprints of RAS imbalance are clearly realized across the frequent organ nervousness and demographic outcomes in COVID-19, suggesting that RAS is the truth is the general denominator.
ACE inactivates the vasodilatory mediator bradykinin, so RAS imbalance would trigger bradykinin depletion, the foundation of the COVID-19 bradykinin hypothesis. And though a latest witness did no longer salvage elevated stages of circulating inflammatory mediators in COVID-19 sufferers, evidence from the hypertension realm suggests that tissue RAS is more principal than circulating RAS for organ procedure nervousness and tissue stages of RAS and cytokines are now no longer as easily quantified in humans.
Resulting from this fact, the evidence suggests that ameliorating RAS imbalance, by strategy of ACE inhibitors or angiotensin receptor blockers, needs to be the pressing focal point of more frequent clinical trials.
There are multiple ongoing or planned ACE inhibitor and angiotensin receptor blocker trials, nonetheless many are taking a watch on the identical agents, as opposed to exploring many different obtainable medication in those lessons. All of these regain sure pharmacologic properties that can also influence capability effectiveness — including some that miserable the blood brain barrier and thus can also affect COVID-19 neurological dysfunction.
As well, recombinant ACE2, entered in one European COVID-19 trial, and an AT2 agonist C21, trialed in pulmonary fibrosis, shall be more widely studied. The vitamin D receptor inhibits RAS on the tissue stage, and African People and older adults more usually show vitamin D insufficiency, so centered vitamin D trials in elevated-likelihood COVID-19 populations can also yield assist.
As COVID-19 continues raging by many ingredients of the sphere, and original outbreaks emerge in areas once deemed under administration, finding the draw to blunt the mechanism of COVID-19’s destructiveness grows easiest more pressing. Evidence suggests RAS imbalance is that mechanism.
We already occupy pharmacological instruments to squash ACE axis overactivity; we must restful use them all.
Maureen E. Czick, MD, is a board certified anesthesiologist and became beforehand an adjunct professor of physiology at Central Connecticut Bid University. Her prior publications explore the physiologic basis of anesthetic ventilatory depression, and the implications of atrial fibrillation pathophysiology for treatment outcomes. Christine L. Shapter, MD, is a board certified psychiatrist; she is clinical director of Greenbrook TMS, and a graduate advisory board member for University of Saint Joseph, each in West Hartford, Connecticut. Her previous publications explore the hyperlink between psychiatry and cardiac illness. Robert Okay. Shapter, MD, is board certified in family medication. He served as a doctor in the Canadian Air Force before transitioning to work for the U.S. pharmaceutical alternate. Shapter beforehand chaired the Household Medications Residency Program at Middlesex Clinic in Middletown, Connecticut, and has been a clinical author and editor for 4 decades.